colonic ischemia vs small bowel ischemia
- related: GI
- tags: #GI
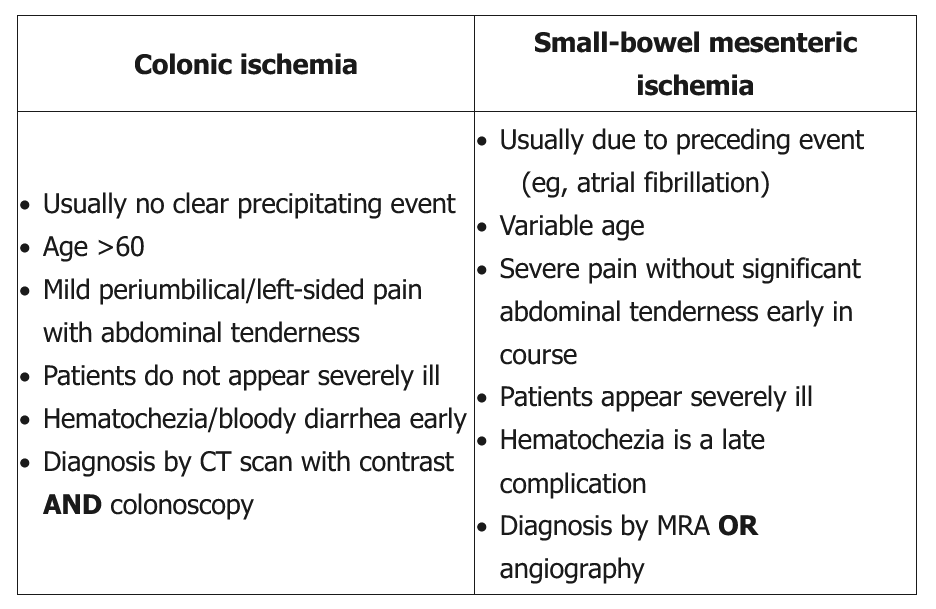
This patient's presentation of acute-onset abdominal pain and hematochezia is typical for colonic ischemia, the most common form of ischemic bowel disease affecting the elderly. Colonic ischemia is usually due to hypovolemia or decreased effective arterial blood volume, leading to an abrupt and temporary decrease in blood flow to the watershed areas (eg, splenic flexure, rectosigmoid colon). Hemodialysis, myocardial infarction, major vascular surgery, strenuous exercise (eg, long-distance running), or drugs (eg, diuretics) can increase the risk of ischemic colitis.
Abdominal CT scan with intravenous contrast is preferred (including in anuric patients on hemodialysis) to rule out extensive bowel damage indicating the need for colonic resection. However, imaging may show nonspecific findings. Colonoscopy (without bowel preparation or air insufflation to prevent perforation) is usually done subsequently to confirm the diagnosis of ischemic colitis. It may show pale mucosa with petechial bleeding, bluish hemorrhagic nodules, or cyanotic mucosa with hemorrhage.
Because most cases of colonic ischemia are nonocclusive, MR angiography is not useful for diagnosis due to the low possibility of finding a thrombus or embolus. Moreover, gadolinium contrast dye should not be used in patients with significant renal impairment due to the risk for nephrogenic systemic fibrosis.